Abstract
Introduction: Patients treated for hematological malignancies are susceptible to life-threatening complications, mainly infections. Prevention of infections and their related mortality presents a major ongoing challenge. The cost of dedicated inpatient services provides an incentive toward early discharge of hospitalized patients. In some high-risk cases (e.g., induction for acute leukemia), the common practice is to admit a patient for observation after completing chemotherapy. However, due to a shortage of dedicated facilities, such patients are often admitted to general internal wards. For ambulatory patients presenting with acute infection, pre-hospitalization emergency care is provided by either a dedicated hematological emergency service or general emergency department (ED). This study is aimed to assess effects of admission to specialized inpatient units versus general wards/ED on infection and death hazards in patients with hematological malignancies.
Methods: This retrospective observational study analyzed data of all consecutive patients with hematological malignancies, treated at a large tertiary center between 01/2011-10/2015. We developed an algorithm allowing accurate identification of infectious events using electronic medical records. In addition to infection diagnosis codes, patient vital signs, and antibiotic prescriptions were included in the analysis to identify poorly recorded events. We assessed infection rates post chemotherapy and infection-related mortality in correlation with the hospital unit where the treatment was given.
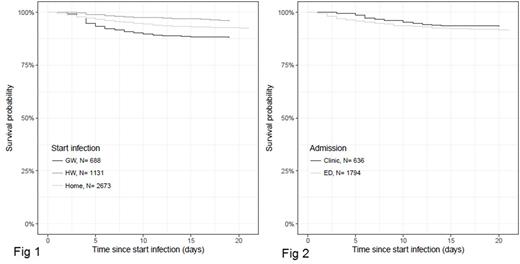
Results: The following outcomes were evaluated: hazard rates of infection within 30 days after completion of the treatment protocol and mortality from an infection. Of 8,786 patients that visited the hematology department, 2,330 received a total of 15,144 chemotherapy cycles within the study period. Excluded from the analysis were 523 cycles where an infection was diagnosed prior to or during chemotherapy administration as well as 2,205 cycles with significant missing data. Excluded were also 1,092 cycles prescribed during the first months after bone marrow transplantation, in which we couldn't differentiate between high-risk patients who received treatment for relapsed/refractory disease and low-risk ones receiving preplanned maintenance/consolidation therapy. The analysis included 11,324 therapeutic cycles given to 1,675 patients [mean age 58.2 years, 47% females, 328 (19.6%) acute leukemia, 119 (7.1%) chronic leukemia, 951 (56.8%) lymphoma, 280 (16.7%) multiple myeloma (MM)]; 88% of cycles were administered on an outpatient basis. Overall, 1,050 infectious events were identified within 30 days after chemotherapy. Patients admitted after chemotherapy conclusion for observation in a general ward had a significantly higher infection hazard rate than those admitted to the designated hematology unit (p-value <0.001) (fig 1). A total of 4,492 infectious episodes, were identified in 1,699 patients during the study period, including events occurring later than 30 days period following therapy. Patient mean age was 57.3 years, 43% were female, 539 (31.7%) had acute leukemia, 163 (9.6%) chronic leukemia, 697 (41%) lymphoma, 303 (17.8%) MM. The primary response to infection symptoms was given through the ED in 1,794 (40%) events. The mortality hazard rate was significantly higher in these patients than in those receiving emergency anti-infection treatment at the walk-in hematology outpatient unit [636 (14.2%), p-value <0.001] or in patients diagnosed with infections while hospitalized [1,131 (25.2%), p-value <0.001] (Fig 2). A patient-specific tool for calculating daily infection hazard risk after chemotherapy and infection-related mortality based on patient characteristics and location was created (available at: https://u0092023.shinyapps.io/InfectionHazards2/ and https://u0092023.shinyapps.io/Mortality/, respectively).
Conclusions: In the current study, patients hospitalized for observation in a general ward had an increased infection hazard compared to those hospitalized in a designated hematology ward. Survival of patients, first treated for their infection at the walk-in hematology outpatient unit, was superior to that observed in patients treated in the ED and even to those who developed infection while being hospitalized for observation in general wards.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal